Introduction to guided tissue regeneration
The ultimate goal of periodontal therapy is to restore the periodontal health and regeneration of the lost periodontal structures. The conventional non-surgical and surgical periodontal therapies lead to the cessation of the active periodontal disease, but in most cases, they result in repair and not regeneration or new attachment. New attachment describes new cementum formation with inserting collagen fibers on a root previously denuded of its periodontal ligament 1. Periodontal regeneration is differentiated from the new attachment in that it must include new bone formation. Studies have established that healing after conventional periodontal therapy includes the formation of a long junctional epithelial attachment 2.
As already discussed in “History of periodontal regenerative therapy”, 1970’s and 1980’s can be considered as two decades when research work enlightened the basic fundamentals of periodontal regeneration. Studies done during this period aimed at discovering whether any of the periodontal tissues (periodontal ligament, alveolar bone or gingival connective tissue) possessed the capacity to regenerate the lost periodontal structures by the formation of the new attachment. Melcher (1976) 3 put forward the hypothesis according to which, certain cell populations residing in the periodontium have the potential to create new cementum, alveolar bone, and periodontal ligament, provided they have the opportunity to populate the periodontal wound. These progenitor cell populations can be derived from four sources,
Epithelial cells
Cells derived from gingival connective tissue
Cells derived from alveolar bone
Cells derived from periodontal ligament
Research work done by Polson and Caton (1982) 4, Lindhe et al. (1982) 5, Karring et al. (1980) 6, Nyman et al. (1980) 7, Karring et al. (1985) 8, Nymen et al. (1982) 9 and Warrer et al. (1993) 10 clearly showed that new connective tissue attachment occurs from cells originating from periodontal ligament. The development of “guided tissue regeneration” (GTR) was aimed at selectively guiding the tissue regeneration in periodontium. The technique of using a barrier to selectively guide the tissue regeneration was first introduced by Nyman et al. 9 in 1982 and the term GTR was coined by Gottlow et al. 11 in 1986. This procedure was also referred to as …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Evidence of attachment gain after guided tissue regeneration
The research work done by the above-stated researchers acted as a foundation for building evidence for the effectiveness of GTR in achieving attachment gain. After it was demonstrated that cells for periodontal regeneration originate from periodontal ligament, a lot of research work has been done on intrabony and furcation defects, using various barrier membranes. A review, given by Needleman et al. (2001) 18 highlights various clinical studies which demonstrate clinical attachment gain after GTR for periodontal infrabony defects. Another systematic review given by Murphy and Gunsolley (2003) 19 on the treatment of periodontal intrabony and furcation defects clearly demonstrates clinically significant attachment gain after GTR procedure. Karring et al. (1993) 20 in a review article have enumerated various animal and human studies …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
A meta-analysis analyzed studies comparing simple open flap debridement with GTR and GTR + bone graft in class II maxillary and mandibular furcation defects. The authors concluded that GTR and GTR + bone graft groups obtained a greater furcation closure rate, vertical/horizontal bone fill, and vertical/horizontal attachment level gain than the open flap debridement group in mandibular molars. The GTR group obtained greater vertical/horizontal bone fill and vertical attachment level gain than the open flap debridement group in maxillary molars. The GTR + bone graft group achieved better clinical outcomes than the GTR group did in all the comparing outcomes in mandibular molars 22.
In another evidence-based treatment approach, Machtei et al. (1995) 23 have reported that …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Biological basis of guided tissue regeneration
The GTR is based on the concept of selective growth of cells derived from periodontal ligament by placing a physical barrier which prevents the apical migration of the epithelium and gingival connective tissue cells along the root surface. Along with this, the physical barrier is also thought to provide protection to the blood clot during early phases of wound healing and ensures space maintenance for the ingrowth of newly formed periodontal apparatus. The barrier membrane has no biological effect on wound healing and proliferation and migration of the mesenchymal and periodontal ligament cells. It must be remembered that GTR procedure cannot be done in all kinds of bone defects and it has specific indications.


Ideal requirements of barrier membrane
Although no membrane used so far for GTR purpose is ideal, but there are some basic requirements that a barrier membrane should possess:
Biocompatibility:
It should be biocompatible. The interaction between the membrane and host tissue should not induce any adverse immunogenic reaction;
Space-making:
It is the ability of the membrane to maintain the space for the migration of cells from periodontal ligament tissue for a stable duration of time.
Tissue integrity:
The membrane should have tissue integrity, i.e. tissue should grow into the membrane without completely penetrating it all the way through. If the membrane does not integrate with the tissue, the epithelium may grow downward on the surface of the membrane to encapsulate it. Tissue integration also provides stability to the overlying flap.
Cell-occlusiveness:
It should prevent the fibrous tissue from invading the defect site, which can delay the bone formation.
Mechanical strength:
It should have enough mechanical strength to allow and protect the healing process, including protection of the underlying blood clot;
Degradability:
It should have adequate degradation time, which matches the regeneration rate of bone tissue to avoid a secondary surgical procedure to remove the membrane.
Membrane configuration and design:
The membrane should be provided in a configuration and design which easily adapts to the defect or it can be easily trimmed for the same.
Indications of guided tissue regeneration
GTR is indicated in the following conditions,
- Two or three walled vertical, interproximal and circumferential intrabony periodontal defects.
- Class II furcation defects.
- Class III furcation defects with less predictability of success.
- Treatment of gingival recession.
- Ridge augmentation (Guided bone regeneration).
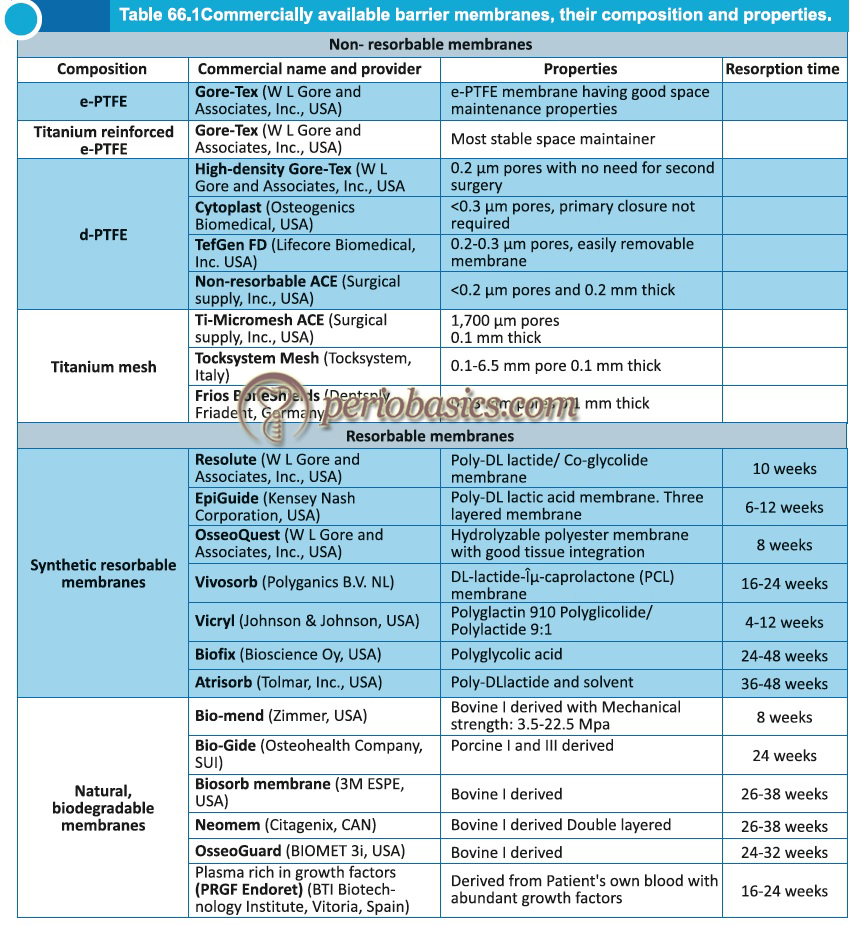
Classification of barrier membranes
The barrier membranes can be broadly divided into non-resorbable/resorbable and natural/synthetic. Following figure describes the classification of barrier membrane.
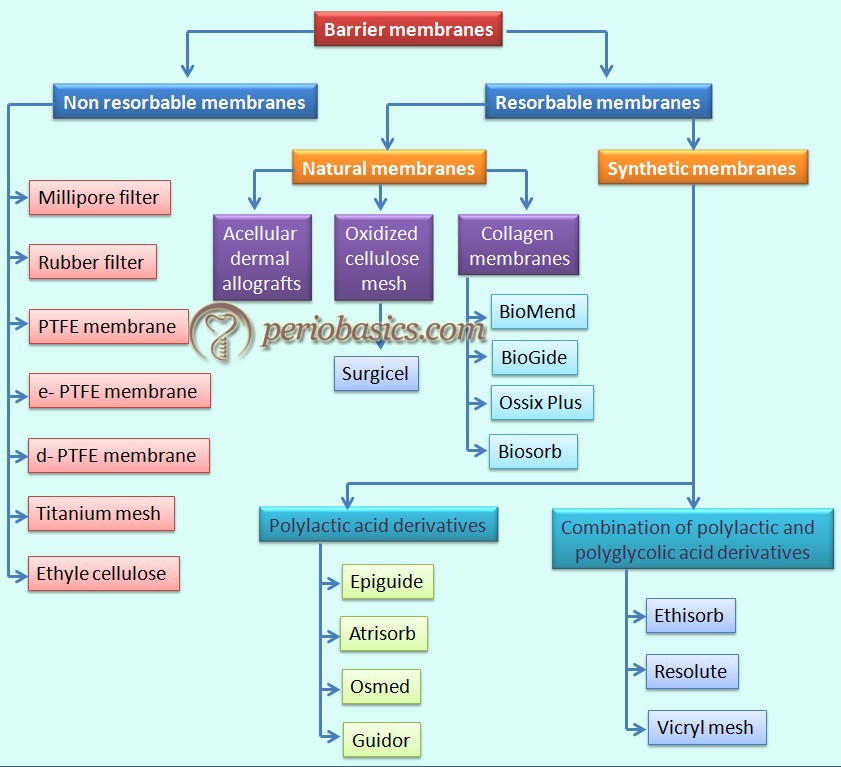
Non-resorbable membranes
The initial barrier membranes used were non-resorbable. These were made up of methylcellulose acetate (Millipore, Bedford, MA, USA). The problem with these membranes was their fragility. They used to tear easily while manipulation, which limited their clinical use. Soon these were replaced by expanded, high-density and titanium-reinforced ethylene polytetrafluoroethylene [ePTFE (e-, d-PTFE and Ti-e-PTFE)] membranes and titanium mesh (Ti-mesh) 24.
Polytetrafluoroethylene (PTFE) membrane:
PTEF membranes were introduced in the dentistry in 1984. This membrane is composed of a biocompatible synthetic polymer with a long carbon backbone to which fluorine atoms are attached. There is no known enzyme in the body capable of cleaving the carbon-fluorine bond. The membrane has a tortuous pore structure. Both surfaces of the membrane have different properties. The outer surface of the membrane has an open microstructure collar of 1 mm thickness and 90% porosity which retard the growth of the epithelium during the early wound healing phase. The inner surface has a 0.15 mm …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….

The surface of the PTFE membrane is rough, which facilitates bacterial adhesion. So, after placement, no surface of the membrane should be exposed to the oral cavity. The main disadvantage of using non-resorbable membranes is the requirement of a second surgical intervention to remove the barrier, 4 to 6 weeks after implantation. It causes trauma to the newly formed tissue and also flap elevation results in a certain amount of crestal bone resorption 25.
To address this problem, a membrane made of high-density polytetrafluoroethylene (dPTFE) was designed especially for use in socket grafting by Bartee and Carr (1995) 26. The surface of this membrane is comparatively smoother and impenetrable by bacteria which does not facilitate the bacterial adhesion or invasion. So, primary closure is not required. After tooth extraction the socket is filled with bone graft and the membrane is placed to cover the opening of the filled socket with its …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Titanium mesh:
It is a suitable alternative for PTFE membrane. Effectively used in guided bone regeneration procedure, titanium mesh has exceptional properties of rigidity, elasticity, stability and plasticity. Rakhmatia et al. (2013) 24 described four main advantages of Ti-mesh membranes over their alternative PTFE membranes:
- These have mechanical properties (rigidity), which makes them suitable for space maintenance.
- The elasticity of the framework prevents mucosal compression.
- Stability prevents graft displacement.
- Plasticity permits bending.
The main disadvantage of using titanium mesh is stiffness of the material and a more complex surgery is required to remove the mesh.
Bioresorbable membranes
Bioresorbable membranes have been developed to avoid the need for surgical removal. These membranes can be broadly divided into two categories: natural and synthetic membranes. Natural membranes are made of collagen or chitosan, whereas synthetic membranes are made up of aliphatic polyesters, primarily poly (glycolic acid) (PGA), poly (lactic acid) (PLA), poly (ε-caprolacton) (PCL) and their copolymers 21. The main problem associated with the use of these membranes is their unpredictable resorption time and degree of degradation.
Natural bioresorbable membranes:
Collagen membranes:
Collagen is the major insoluble fibrous protein in the extracellular matrix and in connective tissue. It is one of the most abundant proteins in the connective tissue. Most abundant collagens in the body are Type I, Type II and Type III. These have a well defined triple helical structural configuration. Collagen Type I polymerizes to form aggregates of fibers and bundles. Collagen remodeling is a …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….



Properties of collagen membrane which make it useful as a barrier:
- It is a natural component of the periodontal tissue, so is well tolerated.
- It is a weak immunogen with the favorable tissue response.
- The collagen membrane is malleable, so can be shaped and manipulated 28.
- Collagen membrane is semi-permeable, allowing nutrient passage and gas exchange.
- Collagen possesses hemostatic properties through its ability to aggregate platelets 29.
- Collagen membrane supports cell proliferation via its lattice structure and cell binding domains.
- Collagen membrane facilitates early wound stabilization and maturation.
- Collagen is chemotactic for fibroblasts 30, 31.
- Collagen membrane promotes cell migration thereby promoting primary closure.
- Collagen membrane is absorbed naturally and if it is replaced by host tissue, volume can be increased.
Collagen is a weak immunogen and its immunogenicity is due to telopeptide non-helical terminals which can be removed by enzymes such as pepsin, producing atelocollagen. One major problem associated with the use of collagen membrane is the rapid degradation of the membrane. The degradation time of the membrane should approximate the healing of periodontal apparatus. To overcome this problem, cross-linked collagen membranes were developed. Cross-linking has been achieved by …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Rothamel et al. (2005) 32 studied the degradation time of various cross-linked and non cross-linked collagen membranes on a rat model. Commercially available collagen membranes Biogide®, BioMend®, BioMendExtend®, TutoDent® and Ossix™ were investigated. They reported that non cross-linked collagen membrane (Biogide®: porcine Type-I and Type- III collagen) had very good compatibility with the host tissue. A rapid vascularization and tissue integration caused their early degradation nearly within 4 weeks without any observable foreign body reaction. The cross-linked collagen membrane (Ossix™) …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Some commercially available collagen membranes:
BioMend® (Zimmer, USA):
This is a collagen Type I membrane manufactured from bovine Achilles tendon. The membrane is semi-occlusive (pore size 0.004 μm) and resorbs in 4 to 8 weeks. The mechanical strength of the membrane varies from 3.5–22.5 MPa. Its fibrous network is proposed to modulate the cell activities, improving healing.
BioGide® (Osteohealth Company, SUI):
This membrane is made up of collagen Type I and Type III of porcine origin. The resorption time is approximately 24 weeks. The mechanical strength of the membrane is up to 7.5 MPa. This membrane is usually used in combination with filler materials.
Ossix Plus® (OraPharma, Inc., USA):
This membrane is made up of Type-I porcine collagen. The membrane has the ability to maintain barrier functionality for 4-6 months, allowing sufficient time for osseous defects to achieve optimal bone regeneration. The membrane has good handling properties and adaptation.
Biosorb membrane (3M ESPE, USA):
This is a Type-I bovine collagen membrane. The membrane is fully resorbed in 26 to 38 weeks. The handling characteristics of the membrane are good. The mechanical strength of the membrane improves its clinical handling due to long, interwoven collagen fibers.
Acellular dermal matrix allografts
Acellular dermal matrix allografts have been used in periodontal plastic surgeries since 1994. As the name indicates, it does not contain cellular material; hence a major histocompatibility complex class I and II antigens are not present in the graft thus eliminating the chances of graft rejection. Other advantages of this membrane include unlimited availability, optimum color matching after healing, acceptable thickness of tissue after …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Amniotic membrane
Amniotic membrane is the innermost layer of the placenta consisting of a thick basement membrane and an avascular stromal matrix. After being harvested, it is kept in a glycerol-preserved, DMSO-preserved or freeze-dried and irradiated state before it is used. This membrane was used for the transplantation of skin in 1910. It has been used in the field of oral and maxillofacial surgery from 1969 onwards, because of its immunological preference and its pain-reducing, anti-microbial, mechanical, and site-dependent adhesive or anti-adhesive properties. It is a composite membrane consisting of the pluripotent cellular element embedded in a semipermeable membranous structure 33, 34. It is tough and lacks blood vessels, lymphatic system, and nerves. Immunohistochemically, collagen Type III, collagen Type IV, and laminin are expressed in the basement membrane of …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book ……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Cargile membranes
These barrier membranes are derived from the cecum of an ox. After isolation, the membrane is subjected to chromatization, similar to suture materials. This procedure prolongs its degradation time and improves the mechanical properties of the membrane. The proposed resorption time of Cargile membrane is 30-60 days. Little data is available regarding the efficacy of these membranes in periodontal regeneration. A study done on dogs using this membrane reported that many sites underwent uneventful healing, significant attachment gain, and bone growth. This study also reported inflammation and resorption of the coronal edge of the membrane in many sites within 2 weeks. The authors concluded that inflammation adversely affects the regeneration of periodontal apparatus 42. The major problem associated with this membrane is difficulty in handling and manipulation during placement.
Oxidized cellulose mesh
Oxidized cellulose mesh is widely used as a hemostatic dressing. It converts into a gelatinous mass upon blood incorporation. It has been reported that this material is absorbed naturally and does not show any harmful effects. There is insufficient clinical data to authenticate the clinical efficacy of this biomaterial when used as a barrier membrane. A study by Galgut (1990) 43 who used this barrier membrane in furcation and interdental …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Chitosan
It is the deacylated derivative of chitin, which is widely used as food preservative. Chitosan is a linear polysaccharide consisting of beta (1-4) linked 2-acetamido-2-deoxy-D-gluco-pyranose (GlcNAc) and 2-amino-2-deoxy-D-glucopyranose (GlcN). These are also referred to as N-acetylglucosamine and glucosamine, respectively. It is routinely derived from the N-deacetylation of chitin from the exoskeleton of marine crustaceans. It exhibits antibacterial and antifungal activity. It possesses hemostatic properties and enhances wound healing and bone formation 44, 45. It is a natural derivative and has a good biocompatibility. The membrane is composed of densely packed Chitosan with optimum handling characteristics. A hybrid membrane containing collagen and Chitosan has been developed by the Central Institute of Fisheries Technology (CIFT), Kochi, Kerala (India), which can be used as a barrier membrane. The resorption rate of this membrane following animal subcutaneous tissue implantation was found to be 12 weeks. The material had a tensile strength of 124 kg/cm2 and a thickness of 0.1 mm.
Freeze-dried dura mater allograft
The freeze-dried dura mater allograft (FDDMA) has been used as a barrier membrane for GTR. This material has been used since 1954 in various fields of surgery, including general surgery, neurosurgery, gynecological surgery and cardio-vascular surgery. In oral surgical procedures, it has been used for vestibuloplasty, mucogingival procedures, repair of oroantral fistula and periodontal regeneration. Since, it is a collagen based barrier, all the properties of a collagen membrane apply to dura mater allograft. One animal study demonstrated an optimal cell occlusive potential of this membrane when used in …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Synthetic bioresorbable membranes
Synthetic materials are widely used for making bioresorbable barrier membranes. They are usually organic aliphatic thermoplastic polymers and, most commonly used materials are poly-α-hydroxy acids, which include polylactic and polyglycolic acids and their copolymers. These were developed by Kulkarni et al. 48 and were originally used in orthopedic surgeries. Magnusson et al. (1988) 49 subsequently used them over buccal dehiscence in dogs and reported a 2.5 mm gain of new attachment above the defect. Since then a lot of research has been done on these membrane highlighting their clinical efficacy.
Upon degradation, the end products of their breakdown are carbon dioxide and water. The degradation may take up to 20 weeks or more depending on their polymeric composition. Although considered biocompatible, a local inflammatory response is associated with their hydrolysis. To what extent this inflammatory response affects the healing process still need to be investigated. Following is a description of commercially available synthetic bioresorbable membranes,
Some commercially available synthetic bioresorbable membranes
Resolute® (W L Gore and Associates, Inc., USA):
It is an occlusive membrane made up of glycolide and lactic copolymer and a porous web of polyglycolide fiber. The occlusive membrane prevents cell ingrowth, and porous part promotes tissue integration. Its resorption time is around 10 weeks. This membrane shows a good integrity with the tissue. The space maintenance with this membrane is good, favoring regeneration. The membrane is degraded via hydrolytic and enzymatic pathways.
Atrisorb® (Tolmar, Inc., USA):
It is the only GTR membrane which is made chairside. It is made up of a polylactic polymer present in the flowable form, dissolved in N-methyl-2-pyrrolidone. When the polymer is exposed to …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Epi-Guide® (Kensey Nash Corporation, USA):
It is made up of a bioresorbable polymer synthesized from D, D-L, L-polylactic acid. The membrane has three layers designed to stop and keep away epithelial cells and fibroblasts. The microscopic structure of the membrane is made up of void spaces which are connected to each other. The membrane is hydrophilic and exhibits good tissue integration properties. The membrane is slowly degraded into CO2 and H2O. The degradation time of the membrane is from 6-12 weeks.
Vicryl Periodontal Mesh® (Johnson & Johnson, USA):
The Vicryl™ (polyglactin 910) woven mesh is prepared from a synthetic absorbable copolymer of glycolide and lactide, derived respectively from glycolic and lactic acids. The membrane loses its structure after 2 weeks and completely resorbs in 4 or more weeks. The membrane is available in four fabricated shapes which can be adapted according to the shape of the defect.
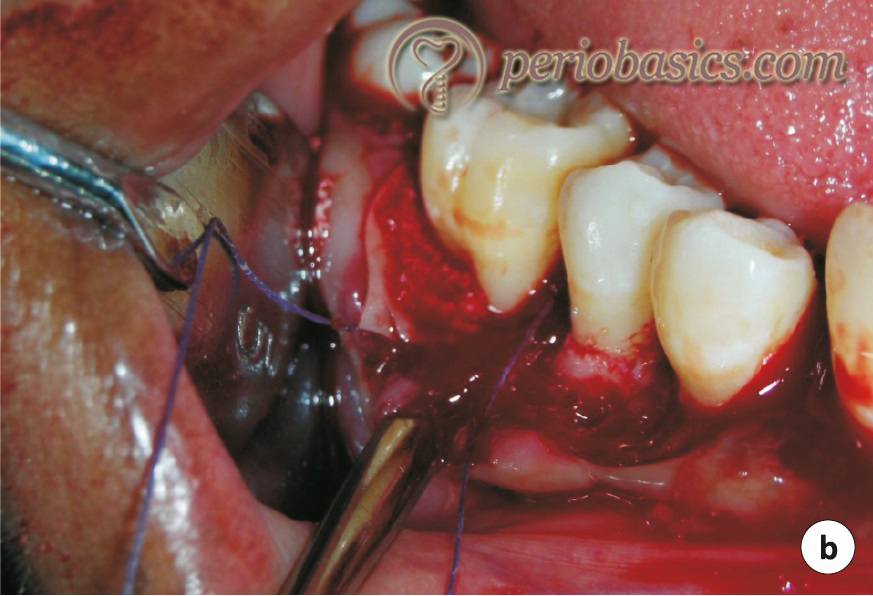
Clinical procedure for guided tissue regeneration
The periodontal bone defects are formed due to periodontitis. The objective of GTR is to regenerate the lost tissue. Before we go for GTR procedure, appropriate treatment for periodontitis should be completed. The following steps are followed during the surgical procedure,
- After achieving profound local anesthesia, the area to be operated is disinfected with an antimicrobial solution such as povidone-iodine, by doing intrasulcular irrigation.
- Sulcular or marginal incision is made and it is extended to one tooth anterior and/or one tooth posterior to the tooth where the procedure is to be performed.
- Vertical releasing incisions are made in such a way that the interdental papillae are preserved.
- Full-thickness flap is reflected and all pocket epithelium is excised from the inner flap surface with the help of sharp curved scissors.
- The granulation tissue present …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
- Make sure that the defect is free of all the granulation tissue and debris. The bony walls of the defect may be decorticated to enhance new bone formation. The rationale behind doing decortication is to facilitate the ingrowth of vessels and bone-forming cells from underlying bone marrow. The defect should be thoroughly irrigated with a normal saline solution before the placement of barrier membrane.
- The scaled and planed root surfaces may be treated with citric acid or tetracycline hydrochloride both of which have a low pH, to remove the smear layer formed due to mechanical instrumentation. It detoxifies the root surface and also exposes collagen matrix of the dentin, thereby enhancing regeneration.
- The selected barrier membrane is carefully taken out of its packing. Many membranes are available in preformed shapes and designs. The configuration most …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
- The membrane should be free of any folds and should adapt close to the tooth surface.
- The membrane is then fixed around the tooth surface using sling suture in such a way that the margin of the membrane is 2-3 mm apical to the flap margin.
- After the membrane is properly secured in its place, the flap is adapted to check the coverage of the membrane. If the margin of the membrane is above its desired level, the membrane should be gently adjusted. Another way of covering the membrane is to give horizontal releasing incision in the periosteum and displace the flap coronally, but it must be done carefully because the horizontal incision may compromise the blood supply of the flap.
- Interrupted sutures are placed to secure the flap in its position.
- The patient is instructed to gently clean the area with a soft toothbrush post-operatively and chlorhexidine (0.2%) mouth rinses are prescribed. The systemic antibiotic is administered immediately prior to the surgery and is continued for one-week post-operatively.
- When the non-resorbable membrane is used, it should be removed 4-6 weeks postoperatively. To remove it, an incision is made starting from the mesial surface of the tooth, posterior to the membrane and extending it to the distal surface of the tooth, anterior to the membrane. The flap is …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
- The patient is instructed to do gentle brushing with a soft toothbrush and is put on chlorhexidine (0.2%) mouthwash for another 2-3 weeks.



GTR procedure for furcation areas:
While doing the GTR procedure in class-II furcation areas, accessibility to the defect is very important. The desired outcome of treating a furcation defect with GTR is the obliteration of the defect by the formation of new bone. The defect is debrided to clean all the granulation tissue and deposits on the root surface. In cases where the furcation is narrow, it may be widened with the help of a flame-shaped diamond stone to get complete access to the defect. The defect debridement, root scaling, root planing and root surface conditioning is done in the same way as described in the previous section. The barrier membrane is …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
GTR is the treatment of choice when class II furcation defects are encountered. However, Novaes and Novaes (1992) 51 listed 8 different situations of class II furcations in which GTR is not indicated:
1. Lack of access for adequate debridement of the furcation area,
2. Endodontic or prosthetic perforations in the furcation areas of the roots,
3. Crown lengthening procedures that invade the furcations,
4. Root proximities untreatable by the restorative alveolar interface technique,
5. Extensive gingival recessions,
6. Deep caries involving the roots,
7. Untreatable endo-perio lesions,
8. Longitudinal root fractures where hemisection is recommended.
Errors which may happen during GTR procedure:
Excessive trauma to the flap:
A full-thickness flap is gently reflected during GTR procedure. Excessive manipulation of the flap may traumatize the flap thereby delaying its healing or it may also cause sloughing of the tissue.
Perforation of the membrane:
If the margins of the bone defect are sharp, they may cause membrane perforation during placement. Any sharp edge of the bone should be smoothened out with minor osetoplasty.
Tearing of the membrane while placing a sling suture:
The bioresorbable membranes become delicate when they come in contact with blood. While placing it around the tooth with the help of sling suture, excessive force may tear the membrane.
Exposed margins of the membrane:
After suturing the flap in its position, no margin of the membrane should be exposed to the oral cavity because it promotes bacterial aggregation and faster membrane degradation. In an animal experimental study, it was demonstrated that in areas with membrane exposure, large inflammatory infiltrate and necrotic tissue were found even when the animals received systemic antimicrobial therapy and daily rinses with a chlorhexidine gluconate solution 52.
Wound healing following GTR procedure
The basic cellular and molecular events that take place during wound healing after GTR are essentially the same as that of wound healing in any other non-oral site. As with any injury, clot formation is the first event that takes place. The main functions of the clot are; protection of the denuded tissues and serving as a provisional matrix for cell migration 53. After clot formation, within a few hours, the early inflammatory response is initiated with the recruitment of inflammatory cells (predominantly neutrophils and monocytes). These cells clean the wound by releasing their enzymes and reactive oxygen species and also by phagocytosis. Within three days …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
In GTR, our main focus is to find out the regeneration of new periodontal apparatus. Studies have demonstrated a lack of mechanical stability of the wound 54 and lack of root surface-adhering fibrin clot 55 as the main factors in the formation of a long junctional epithelium instead of the new attachment formation. To systematically study the periodontal regeneration following additive procedures like GTR, Koo et al. (2004) 56, 57 developed a preclinical model, designated as the “Critical-size supra-alveolar periodontal defect model”.
In this animal model, the periodontal defect was made in such a way that regeneration could not take place without adjunctive methods. They surgically removed the alveolar bone and periodontal attachment, including the cementum, circumferentially around the third and fourth mandibular premolar teeth to a level 5-6 mm from the cementoenamel junction. This model was then subjected to various clinical investigations. In their first study, they investigated the …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
In subsequent studies, they covered the heparin treated root surface with polylactic acid or expanded polytetrafluoroethylene (ePTFE) membranes. Connective tissue formation rather than long junctional epithelium was demonstrated in these areas showing the importance of wound stability and space maintenance 59, 60. One study evaluated regeneration in the absence of strict cell occlusion 61. A tissue expanding gold mesh was applied in surgically created horizontal periodontal defects in the mandibular premolar region in dogs. The contralateral defect served as control which was closed without gold mesh. The results of the study demonstrated new bone formation in test sites as compared to control sites, demonstrating that new bone formation may proceed in the presence of space without strict occlusion of the gingival connective tissues.
Factors affecting periodontal regeneration
Defect morphology:
As explained in “Patterns of bone destruction in periodontal diseases”, the periodontal bone defects can be classified as one wall, two wall, and three wall defects or their combination. This classification indicates only the bony wall remaining around the tooth and does not indicate about the status of the periodontal ligament. The cells for regeneration are derived from the remaining periodontal ligament space. In general, more the walls of the bone remaining around the defect more is the periodontal ligament space surrounding the diseased root surface. For example, in a three-wall bone defect, the diseased root surface is surrounded by periodontal ligament from three aspects. Thus, the chances of the formation of new attachment are highest for three wall defect and least for one wall defect. In other words, we can say that more is the ratio between remaining and lost periodontal ligament, more are the chances of regeneration.
Innate regenerative potential:
Innate regenerative potential varies from individual to individual. In some patients, the results of periodontal regenerative therapy are as desired, while in others they are not, in spite of an accurate surgical procedure. This can be explained on the basis of the innate regenerative potential of an individual.
Surface topography and porosity of barrier membrane:
The pore size of the barrier membrane is important because it should prevent excessive penetration of fibrous tissue into the bone defect (soft tissue ingrowth) but at the same time, it should allow neovascularization and bone formation. It has been shown that a pore size more than 100 μm is required for the penetration of highly vascular connective tissue. If the pore size is less than 100 μm, primarily avascular tissue grows because the pores are inadequate for penetration of capillaries. A study has shown greater bone formation with macroporous membranes as compared to microporous membranes 62. But, increasing the …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Mechanical stability of the membrane:
Any kind of micro movement in the membrane adversely affects the healing process and prevents bone formation. In most cases, it results in fibrous tissue formation 63, 64. It has been shown that for early tissue growth and bone formation, adequate stability and minimum stress are the prime requirements 62. Along with this, minimal inflammation provides a conducive environment for adequate vascularization of the healing area thereby promoting regeneration. Since most of the resorbable membranes are flexible, it is difficult to stabilize them around the defect. To maximize the stability of these membranes, use of membrane-fixing pins has been suggested. It should be noted that while securing the membrane with suture in place, care should be taken not to put undue pressure on it which may lead to membrane rupture.
Soft tissue ingrowth in the membrane:
The barrier membrane is an occlusive membrane, not allowing ingress of any kind of cells or soft tissue. A thin layer (up to 1 mm thickness) of soft tissue may be formed under the membrane which may be due to shrinkage of the initial blood clot under the membrane, entrapment of air or membrane micromovements. The clinical significance of this soft tissue layer is not known.
Stabilization of blood clot:
Stabilization of the blood clot is the primary requirement for GTR success. The defect should be free of all granulation tissue and soft tissue. The membrane should extend 2-3 mm beyond the defect so that any migration of the epithelium and soft tissue below the membrane should be prevented. While flap closure it should be …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Tooth mobility:
Tooth mobility may adversely affect the healing process, mainly due to the fact that wound stabilization is a primary requirement for healing. Hypermobile tooth may jeopardize the clot stability, hence healing. The membrane attached to a hyper-mobile tooth moves along with the tooth thus compromising flap healing. Hypermobility may temporarily increase after surgery, causing discomfort to the patient. keeping all these factors in mind, the hypermobile tooth/teeth should be splinted before performing GTR procedure.
Patient-related factors:
A patient scheduled for GTR procedure should be well motivated and should have undergone a thorough hygienic phase of treatment. The patient must maintain a good oral hygiene during the healing period. Any inflammation of tissue surrounding the membrane causes early degradation of the membrane, thus resulting in partial or complete failure of GTR procedure.
Cigarette smoking has been associated with a reduced healing response following GTR treatment 23, 65, 66. It has been shown that the most significant effects of smoking on periodontal healing occur during tissue maturation phase 65, 66. It has been suggested that when GTR treatment is done for class II furcations in smokers, an anti-infective therapy should be incorporated into the treatment protocol to enhance the regenerative outcome 66.
Stress is another patient-related factors which may adversely affect the outcome of GTR therapy. The proposed mechanism of negative effects of stress on healing after GTR therapy are, neglect of oral hygiene, changes in diet, increase in smoking and other pathogenic oral behaviors, bruxism, alterations in gingival circulation, changes in saliva, endocrine imbalances and lowered host resistance 67.
Systemic conditions like diabetes mellitus also adversely affect the outcomes of GTR therapy. Susceptibility to periodontal microbial colonization and impaired wound healing after surgical therapy …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Recent advances in GTR membranes
As already discussed, the traditional membranes used in GTR procedure include the resorbable and non-resorbable membranes. There have been many recent advances in the development of the membranes in an effort to enhance the regeneration that we can achieve following GTR procedure. Various attempts have been made to combine the biomaterials to achieve the right combination of mechanical, degradation, and biological characteristics required for guided tissue regeneration. Furthermore, various biologically active molecules have been added in the membranes to achieve maximum periodontal regeneration. Various advancements in the formation of GTR membranes have been done using tissue engendering. These advancements are,
Membranes with therapeutic properties:
The most common cause of failure of a regenerative procedure is infection. Hence, every attempt should be made to control and/or eradicate bacterial contamination of the periodontal defect 68, 69. Attempts have been made to incorporate various anti-microbial agents in the membranes, including tetracycline hydrochloride, metronidazole, and amoxicillin, etc. In a recent study, Furtos et al. (2017) 70 developed a nanocomposite polycaprolactone (PCL)-based membranes modified with amoxicillin and nanohydroxyapatite to provide antimicrobial and osteoconductive properties, respectively.
However, it should be noted that the use of antimicrobials may be associated with the development of resistant strains of bacteria. Keeping it in mind, various researchers have developed membranes containing alternative agents such as zinc oxide (ZnO) nanoparticles. Recently, the synthesis of PCL based nanofibrous membranes using ZnO has been reported. In this study, the anti-microbial property of ZnO was tested against Porphyromonas gingivalis and Fusobacterium nucleatum. It was demonstrated that ZnO demonstrates significant anti-microbial activity against the tested periodontal pathogens 71.
Membranes with growth factors:
The growth factors are essential components of regeneration. Research has demonstrated that growth factors like BMP-2 84 and PDGF-BB 85 enhance periodontal regeneration by enhancing the regenerative potential of the cells involved in periodontal regeneration. Further PDGF-BB has been shown to promote angiogenesis, which is a very important step in regeneration 85. Phipps and Bellis (2012) 85 synthesized PCL-collagen I membrane incorporated with PDGF-BB and hydroxyapatite nanoparticles. In this study, a sustained release of PDGF-BB was observed for 8 weeks in addition to enhanced mesenchymal stem cell chemotaxis. In another study, Ji et al. (2013) 86 synthesized stromal cell-derived factor-1 (SDF-1α) modified …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Multilayered membranes:
The primary aim of using GTR/GBR membranes for periodontal regeneration is to interfere with the ingrowth of the epithelium and gingival connective tissue and to allow the growth of PDL and alveolar bone cells. As the structural and functional requirements of the membrane are different on the outer and the inner surface, we need to utilize a graded-structure with compositional and structural gradients that meet the local functional requirements. To meet these requirements, fabrication of a functionally graded three-layered membrane from PLGA, collagen, and nano-hydroxyapatite by a layer-by-layer casting method has been attempted 87, 88.
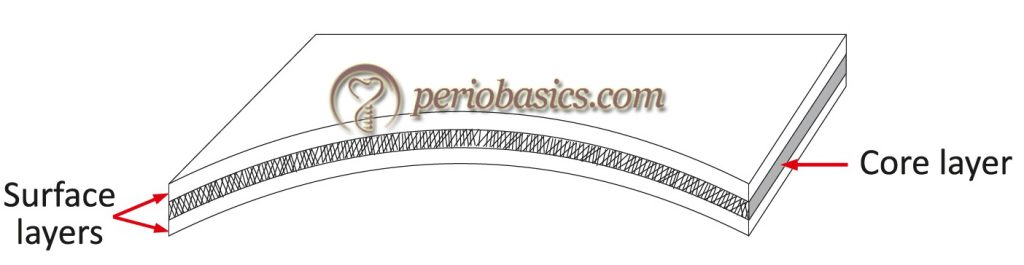
Recently, e-spun functionally graded nano-fibrous tubular scaffolds with distinct chemical compositions as well as tailored degradation and mechanical properties have been developed 89-91. The functionally graded membrane (FGM) is prepared by multilayering e-spinning procedure. The membrane consists of a core-layer (CL) and …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….. Contents available in the book …….
Platelet-rich fibrin membrane (autologous membrane):
The membrane is made up of autologous platelet concentrate. The PRF was first developed in France by Choukroun et al. (2006) 92. A blood sample is taken without anticoagulant in 10-mL tubes which are immediately centrifuged at 3000 rpm for 10 min. The fibrin clot obtained is used as a membrane. The scientific rationale behind the use of these preparations is that the platelets contain α granules which are the reservoir of many growth factors (GFs) that are known to play a crucial role in hard and soft tissue repair mechanism. A detailed description of the procedure has been given in “Application of platelet concentrates in Periodontics”.
Assessment of regeneration
As explained in chapter 65 “History of periodontal regenerative therapy” the assessment of GTR is usually done by one of the few methods. Periodontal probing, radiographic analysis, re-entry, and histological evaluation are the techniques employed to assess the results of GTR.
Conclusion
GTR has evolved as a promising technique for periodontal regeneration. Since the introduction of the concept of GTR, various bioresorbable and non-bioresorbable membranes have been introduced. The bioresorbable membranes are more extensively used today because they do not require a separate surgical procedure for their removal. Although good results can be achieved with this procedure, complete periodontal regeneration is still far. Future research is directed towards developing new techniques to achieve this goal.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

